Nursing Committee Updates
Quality Safety and Care Improvement
The Quality Safety and Care Improvement (QSCI) committee reviewed fiscal year 2010 fall prevention program outcomes and current data. Current fall prevention initiatives include:
Implementing comfort rounds on all units. Units that have already implemented comfort rounds have noted an increase in patient satisfaction scores, as well as a 7.3 percent reduction in falls with injury. This remains a Department of Nursing goal.
Improvement of fall risk communication with a revised transport communication sheet is awaiting approval to pilot.
Implementation of high-risk fall rounds by PCAs at change of shift results in a 50 percent decrease in falls at this critical time.
Creation of a post-fall checklist (not part of the permanent record) guiding nurses in creating a well-documented plan of care and follow-up post fall.
The committee heard presentations from the infection control department highlighting ICU MRSA, VRE, CLABSI, VAP infections results, with a focus on environmental equipment cleanliness. VRE is the most problematic, resulting in the exploration of environmental issues such as high touch equipment, e.g., alarm buttons and surface areas as routes of transmission. Staff are contaminating their hands after cleaning them by touching dirty equipment and surfaces. Infection control is working with environmental services, UCs and PCAs around terminal cleaning of patient rooms with specific focus on equipment and high touch surface areas. Infection control is seeking nursing’s input on how to reinforce appropriate cleaning of unit equipment between patient use to promote consistent, safe practice.
The QSCI committee meets the second Tuesday of every month. Please direct questions to co-chairs Stephanie Capello, RN, and Martha Doherty, RN.
Practice Committee
The Practice Committee continues to explore how we preserve and extend the excellent practice uncovered in the practice of BWH nurses through Finding and Defining the Good.
Recently, the committee has focused on learning more about excellent nursing care from the patient’s perspective. After hearing from a committee member about her perspective when her husband was an inpatient, the committee discussed an article that reported on patients’ perceptions of nursing care. Members shared experiences of getting feedback from patients and families, both positive and negative. The committee asked what it would look like to intentionally seek feedback from patients who are the recipients of nursing care. How would that feedback change practice? The committee will invite a patient and/or family member to a future meeting with the intent of expanding our knowledge and understanding of this important topic.
The committee has determined goals for the next year. The priorities identified by members included supporting narrative development and advancing the knowledge of stages of practice development throughout the Nursing Department. The committee will continue to work hard on identifying a communication plan that will effectively share its learning and engage the entire nursing community in the dialogue about patient care and practice development
If you have questions, contact committee co-chairs Mary Beth Mondello, MSN, CNRN, NP-C, and Alice O’Brien, MS, RN.
Patient and Family Education
The Patient and Family Education Committee worked with the Acute Care Documentation (ACD) team to design the new electronic patient education documentation in ACD. First, the committee defined what they felt were important requirements for the new design. These requirements include the ability to:
- Support documentation of the patient education practice: assessment of learning needs, planning learning goals, teaching interventions and evaluation of learning
Meet Joint Commission requirements
Fit into the nurse’s workflow and be easily accessible
Write a narrative of patient education
Communicate patient education to the health care team
Allow documentation of follow-up teaching on all learning needs
Provide a comprehensive view of all patient education done
Next, a small Patient and Family Education subcommittee collaborated with ACD and Nurse Informaticist, Deb Furlong, RN, to design a prototype based on the above principles. Finally, Furlong presented the patient education prototype to the committee for their feedback and approval. The general consensus of the committee about the new design is best summed up in the comments of the committee co-chairs: “This will be a great improvement!”
Please contact committee co-chairs Deb Moody, RN, and Cindy Loring, RN, with questions.
Informatics and Clinical Innovations Committee:
The Informatics and Clinical Innovations Committee continues to advocate for clinical systems projects to support work of the nurse at the bedside and promote patient and staff safety. Our projects include:
eMAR Updates/Enhancements:
The Newborn eMAR implementation started April 12 in NICU C. Bar coding will be available for both medications and human milk. As a part of this rollout, there are four new enhancements that all nurses will see in eMAR:
Human Milk category / folder on the To Do List
Newborn Reference Tab in eMAR
Expanded Pain Scale Choices
Icon on the To Do List indicating if a female is pregnant or breast feeding
Changes Coming to the Potassium Sliding Scale Orders:
In the next month, new sliding scale potassium orders will allow nurses to administer a one-time dose for K + <3.1 until the ordering clinician is contacted to obtain additional orders.
Information System Downtimes:
There will be an information systems downtime May 16 from 2 to 4 a.m. The informatics committee designed a new cue card with instructions on how to log on to the failsafe computer to access ordering and medication information during the downtime. Cards will be distributed to all staff for reference. Contact your nursing leadership team to obtain a card.
ACD Hardware Update:
Staff nurses on Tower 3BC and 11 are trialing new computers mounted in the patient rooms in preparation for the acute care documentation project. Feedback for this trial will help decide the hardware model for the project.
If you have questions, please contact co-chairs Heidi Smith Doucette, CNRN, or Carol Booth, MSN, RN, PCCN.
Standards Policies and Procedures
The Standards, Policies and Procedures Committee is always trying to find new ways to make the Nursing Clinical Practice Manual more easily accessible. To that end, a new index has been developed with sections listed alphabetically at the top of the page. If you know the section, just click on the link. You can scroll down and click on the policy you are looking for.
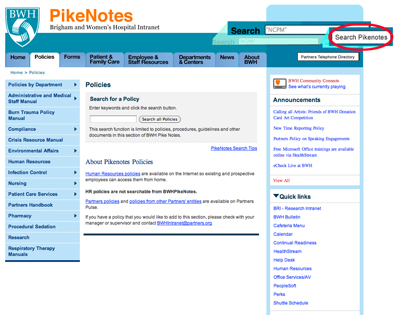
Using the search engine at the top of the PikeNotes page is yet another way to locate specific policies. To avoid generating a list of any policy in any manual that contains the key word, first type in “NCPM” (Nursing Clinical Practice Manual), and then type the key word. This will generate only nursing policies and procedures. Remember you must click on the “Search Pikenotes” tab for this option to work. Since improving the functionality, the number of “hits” per month has increased from 300 to an average of 3,000.
The committee approved changes to the Patient Education Section of the Flow Sheet to improve documentation of patient education. Check boxes have been added so nurses can indicate when additional patient education is documented in other areas of the medical record.
The Flow Sheet Documentation Guidelines also will be updated to give step-by-step instructions on how to document patient education according to The Joint Commission standards.
MED-01 and MED-15 have been updated to reflect a Joint Commission requirement. Medications that are multi-dose are to be labeled with the date of expiration, not the date opened. The committee is aware that this is a huge practice change and is working with other departments to make this easier.
After a review of Joint Commission standards, it was determined that no printed or transcribed lab value reference ranges are to be written on flow sheets or printed and placed in bedside books or charts. Accurate reference ranges are to be obtained online with the lab value.
As always, please send feedback to co-chairs Cindy Jodoin, RN, and Sharon Swan, RN.